“Alzheimer’s epidemic puts advisers – and their practices – at risk” (InvestmentNews.com, February 26, 2013). “Clients with Alzheimer’s pose “scary” legal risks” (InvestmentNews.com, February 13, 2012). “Money woes can be early clue to Alzheimer’s” (New York Times, October 2010). The worry has been there for some time. The problem of risk management is as clear as is the solution.
Alzheimer’s disease unfolds over the course of 30 or so years, progresses slowly, and does not produce disability until well advanced. Progressive dementias unfold like reverse development. First in, last out. We learn walking and talking very early. Managing technology and complex decision-making comes much later. It’s no wonder that complex decision-making, like investing and managing money and legal decisions, are the first signs of decline. It appears to sneak up on us – but it does not.
Alzheimer’s disease gives adequate warning to allow developing a proactive plan that gets ahead of changes and unfolds based on feedback from objective data and self-determination – just like long-term investment strategies and advanced directives. It seems to me that the solution is obvious. We must quit waiting for a medical diagnosis as that puts us in a reactive rather than a proactive stance.. The problem early on is progressive and measurable short-term memory decline. A brain scan or a memory screening, a MMSE, does not detect memory change. Memory change is not a medical problem.
Memory is not solely the domain of medicine. All professionals (i.e., financial, legal, medical) have an obligation to their clients to help them monitor their own memory with objective and quantifiable assessments. As we gather data to set up financial and/or legal estate planning, we owe it to our clients to begin memory assessment as part of the program from the start. We must help clients make their decisions fully informed of how well their memory is working. We need to help them be proactive and act in their own best interests before decline becomes more than just forgetfulness.
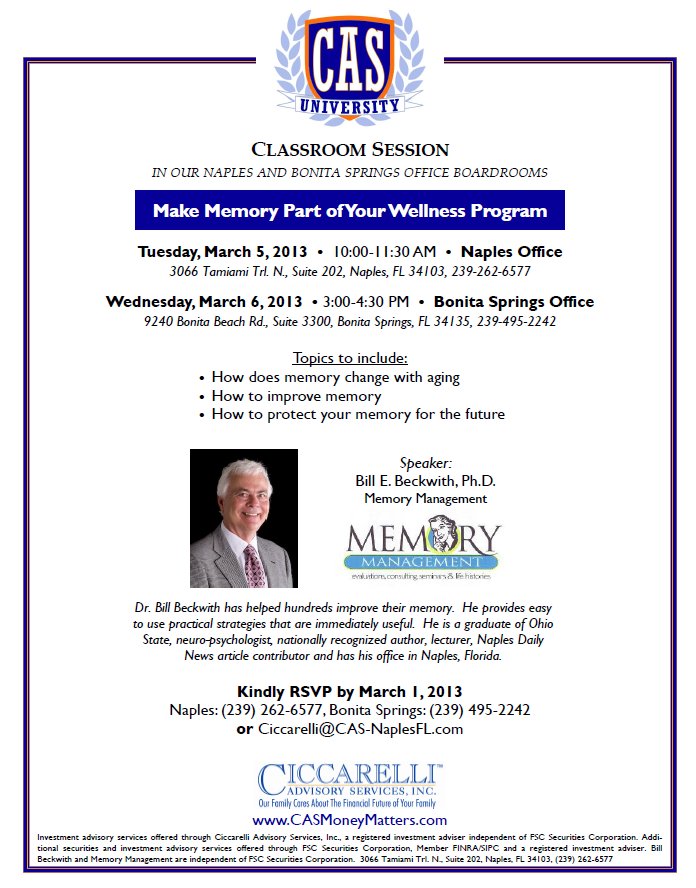
I have been working with Tony Curatolo, Ciccarelli Advisory Services, to develop a plan to better serve his and my clients. As we discussed the many complex issues of detecting decline, it became clear that neuropsychologists are reluctant to discuss money matters and financial advisors are reluctant to discuss memory. We both need to change our practices as our clients are the ones who are getting short changed.
Next week I will outline a simple, proactive plan that may serve as a model.